How to Design Virtual Care Experiences Patients Actually Trust
Virtual care requires its own design principles, product thinking, and understanding of human behavior. Here are some design insights for creating exceptional and trustworthy telehealth experiences.

Virtual care is often treated as a digital substitute for in-person visits. But it’s a distinct medium that demands its own design principles, product thinking, and understanding of human behavior.
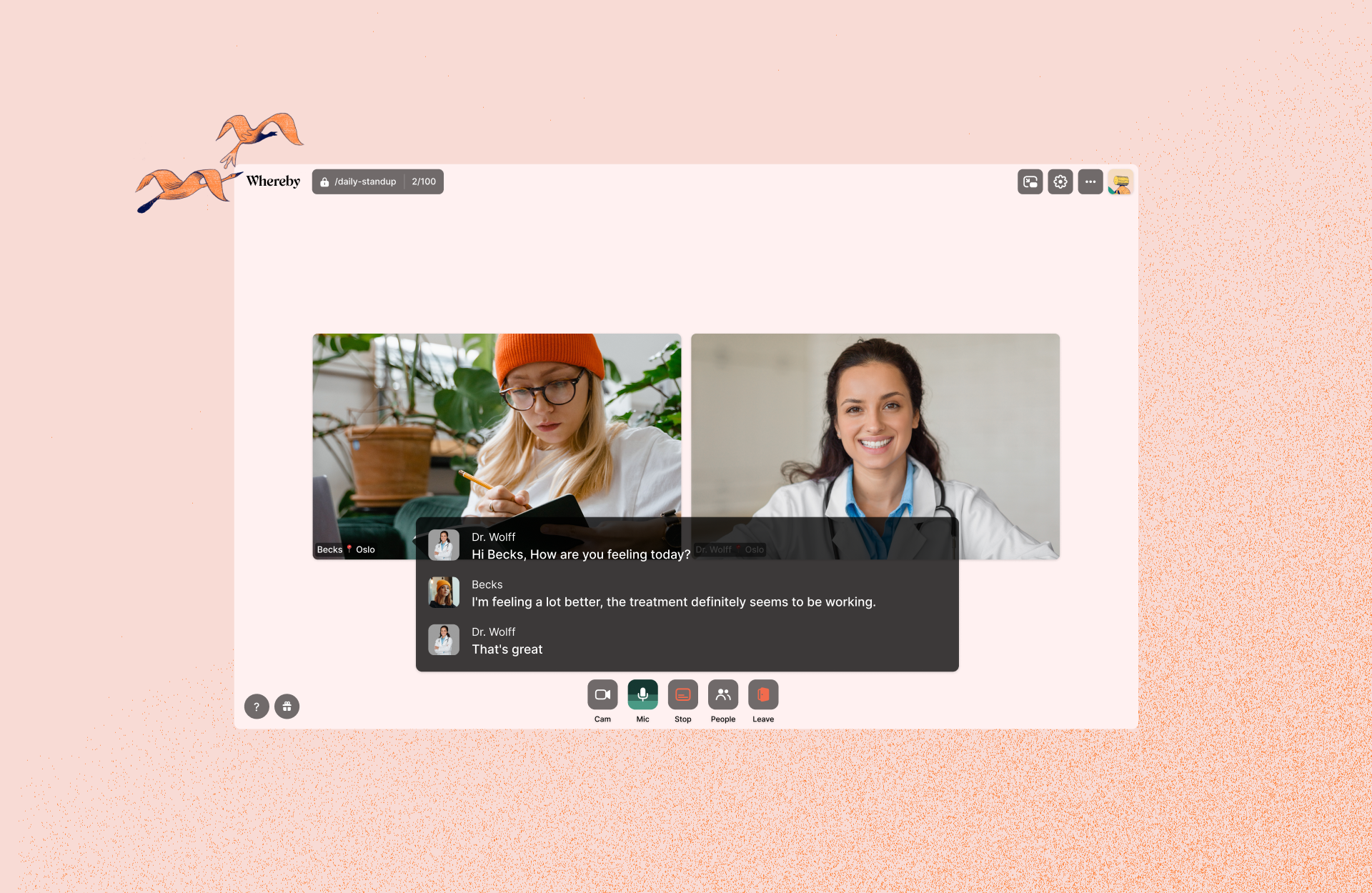
At Whereby, we believe exceptional virtual care is defined by how intuitive the technology behind it is and how it makes people feel.
The right experience builds trust, clarity, empathy, and ultimately leads to better clinical outcomes. A poor UX, on the other hand, drives no-shows, discourages repeat virtual visits, and pushes practitioners to switch to another telehealth platform.
When the virtual care experience is designed well, it feels calm, reliable, and human. When it isn’t, it introduces friction and anxiety at the moment patients need reassurance most.
So in this article, we’ll share design insights for creating exceptional telehealth experiences.
Designing telehealth video sessions
Telehealth environments are fundamentally different from meetings or social video calls.
In healthcare, the stakes are higher, and the margin for error is lower. Patients may be anxious, unwell, unfamiliar with the technology, or all three at once. Practitioners, on the other hand, are working against time, cognitive load, and clinical responsibility.
This influences everything about how the video call experience for telehealth should be designed. Keep in mind that;
The technology should fade into the background, allowing the clinical interaction to take centre stage.
If patients have to think about how to join, where to click, or whether something is working, the experience has already proved to be unintuitive.
So while general video-call environments tend to optimize for many use cases and include a variety of features, virtual care sessions need a refined experience designed specifically for caregiving.
Users want to make fewer decisions, experience fewer distractions, and practitioners want to see fewer opportunities for things to go wrong.
Shaping trust through design
Exceptional virtual care is shaped by moments most people barely notice until it doesn’t work.
The first is when a patient joins a session. This step is particularly important because it sets the emotional tone for everything that follows. So reduce friction as much as possible by eliminating downloads, logins, and unnecessary technical steps.
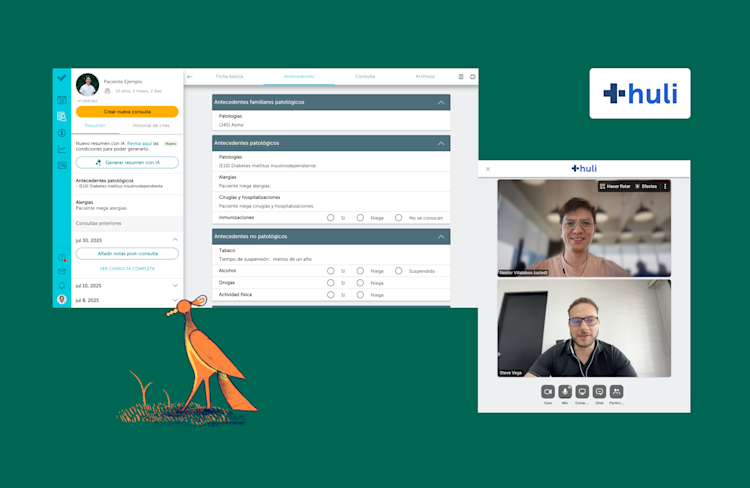
Embed video calls directly into familiar patient environments (via API solutions like Whereby), so patients know they’re in the right place and aren’t pushed out to an unfamiliar third-party experience.
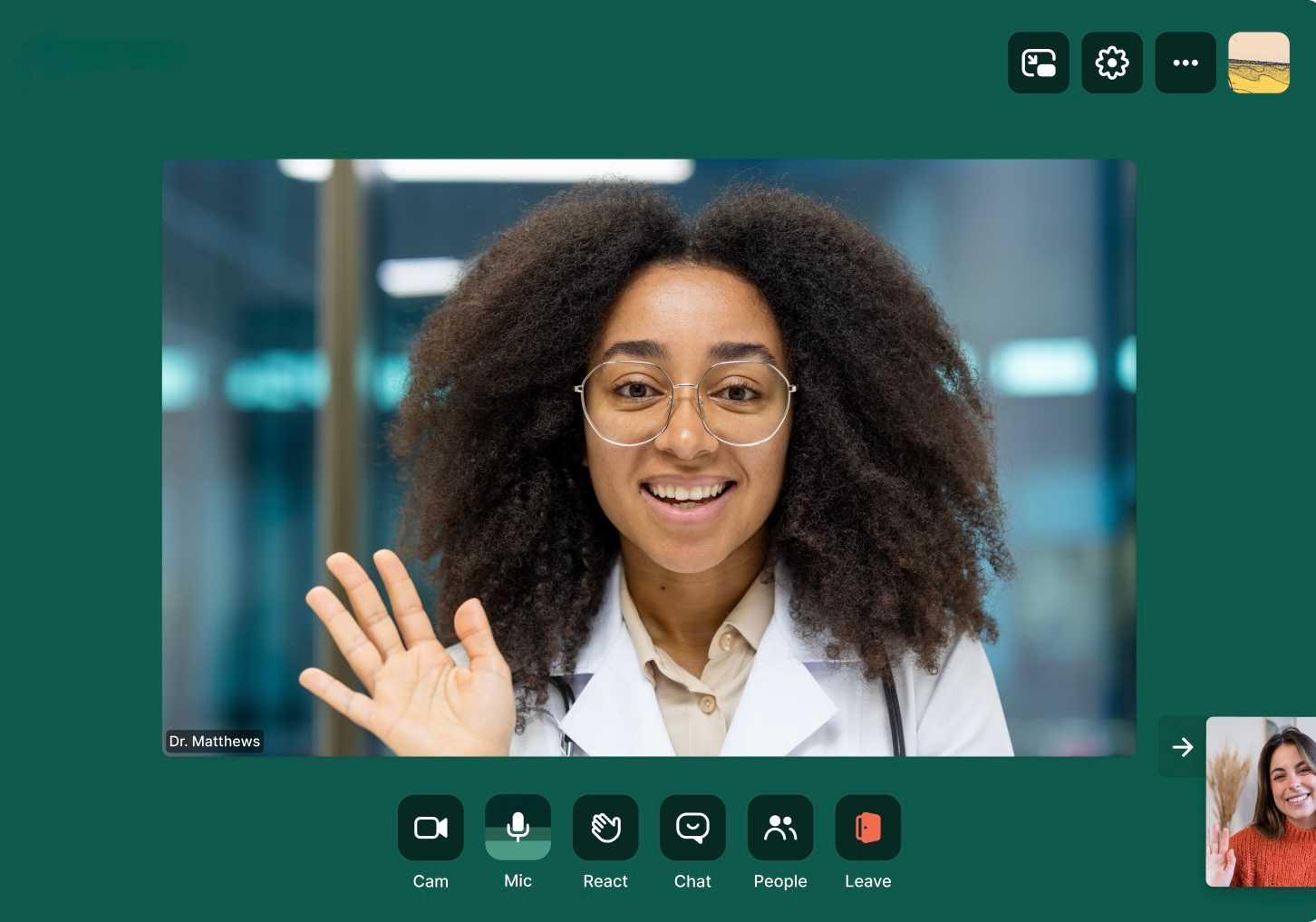
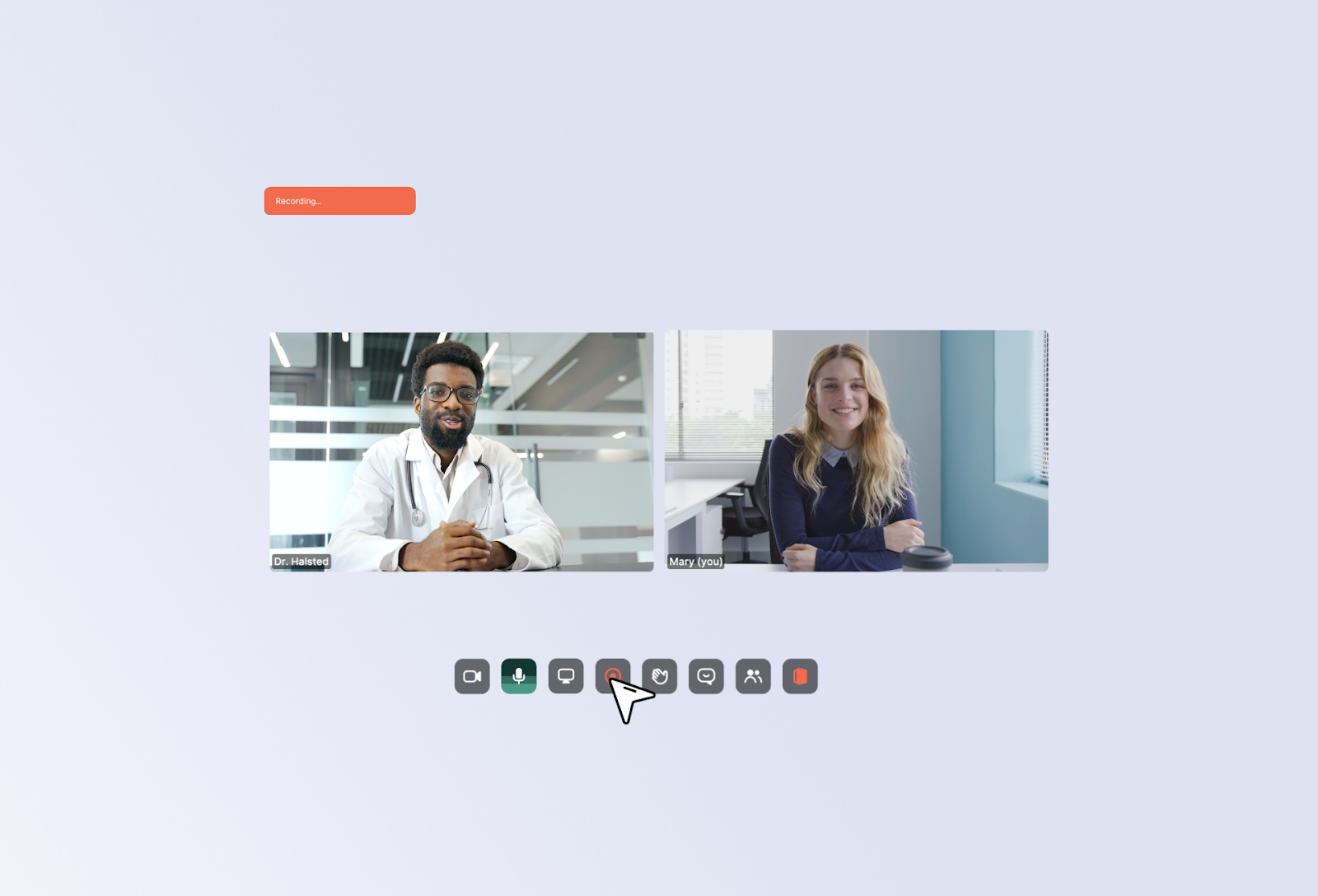
Once the session begins, the in-call experience should feel calm and unobtrusive. Use clean interfaces, simple colour palettes, and minimal, non-distracting controls. Give patients and practitioners clear, reassuring UI cues for actions like recording or transcription, so nothing feels unexpected or confusing.
Thoughtful layouts, clear roles, and intentional transitions in general help to reduce cognitive load and allow both parties (patients and practitioners) to focus on the conversation rather than the interface of the video call solution.
Designing for when things go wrong
No virtual experience is immune to real-world constraints. In fact, in our latest research on the state of virtual care, 91% of telehealth professionals said that they or their users experienced technical difficulties at least occasionally.
So events like low bandwidth connectivity issues, outdated devices, late arrivals, switching devices, or environmental interruptions are inevitable. However, where many virtual care experiences could improve is not in preventing these moments, but in how they respond to them.
Designing for virtual care means assuming things will go wrong and building resilience into the experience without clinicians needing to become tech support.
So think around building a clear system feedback, graceful recovery paths, and guidance to help prevent small issues from escalating into frustration or loss of trust.
For example, on Whereby Embedded, to help resolve hardware and connectivity issues, we introduced pre-call checks. This ensures everyone is fully confident with their camera, mic, speaker and connections before going into a session.
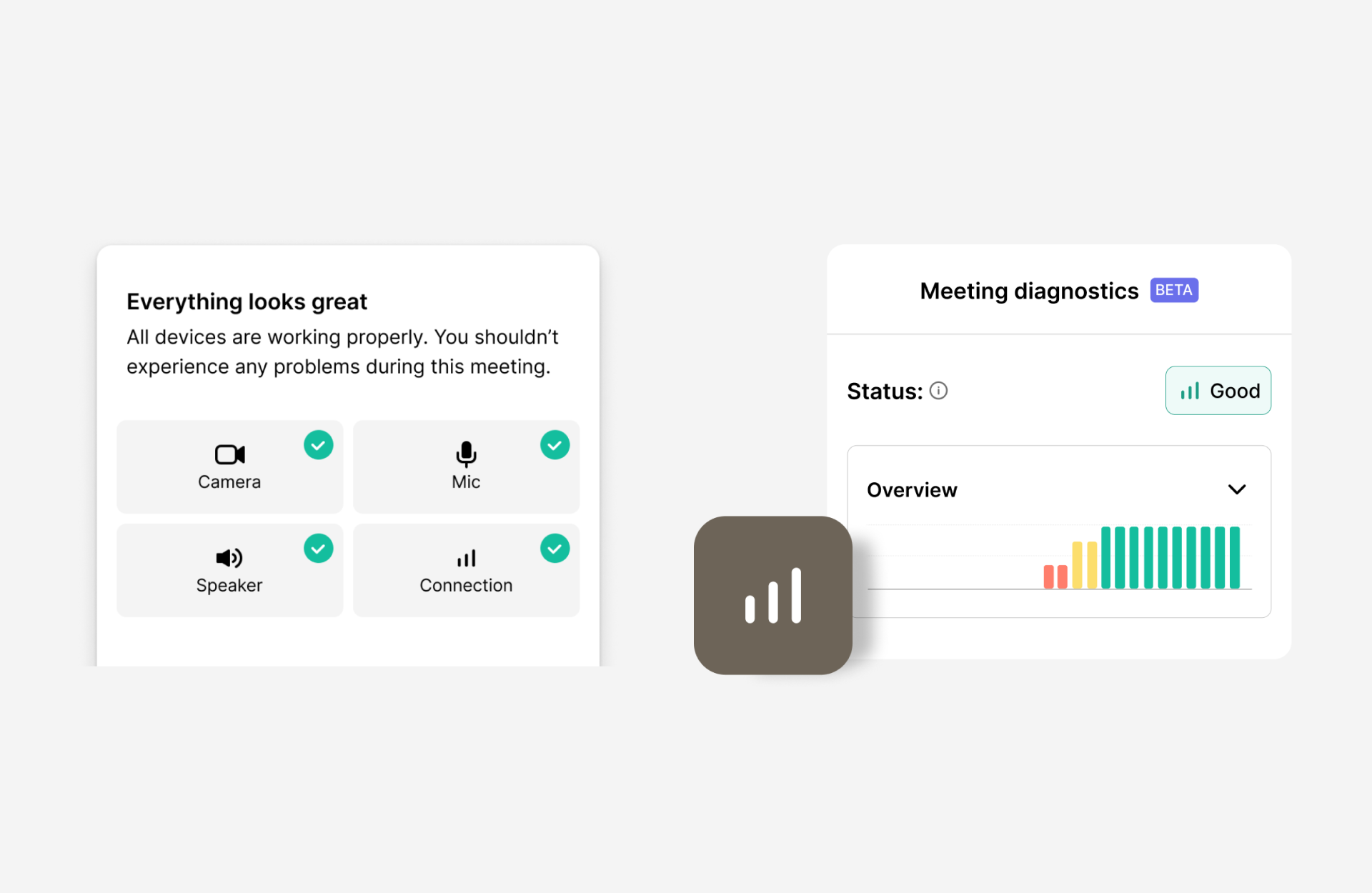
There’s also in-call diagnostics to quickly identify what the issue is if a technical issue occurs mid-session.
Designing for accessibility
Accessibility in virtual care is more than just a checkbox. Over 1.3 billion people globally live with a significant disability, so teams need to prioritize inclusive design.
In virtual care, inclusive design also goes further than formal accessibility standards. For example, patients may be older or less digitally literate. Some might be joining appointments while tired, anxious, or unwell, and using older devices or unstable connections.
Others, particularly in mental healthcare, may need to access sessions from non-traditional safe spaces, such as joining on a mobile phone from a car because it’s their only private environment.
This makes cross-device compatibility, low cognitive load, and resilient performance essential.
Designing for accessibility means reducing steps, simplifying language, supporting assistive technologies, and ensuring the experience works across devices and bandwidth conditions.
Thoughtful features like live captions, transcriptions, keyboard shortcuts and navigation, virtual backgrounds, multiple languages and screen reader support can make all the difference.
At Whereby we believe that everyone deserves equal access to great virtual care, which is why, in addition to our prebuilt UI being WCAG 2.1 Level AA compliant, we’re constantly improving our accessibility options.
Learn more about our accessibility features here.
Designing for human interactions
The goal of virtual care isn’t to perfectly replicate in-person visits, but it should preserve what matters most, which is human interaction.
Human connection still relies on simple gestures like eye contact, facial expressions, a sense of presence, and feeling listened to. So the UI/UX of your telehealth platform plays a direct role in whether a patient feels supported or overlooked.
Thoughtful design often starts with restraint. A minimal toolbar or video call screen reduces cognitive load, helping patients stay focused on the session rather than the UI.
Other design elements like video framing, the layout and visual hierarchy heavily influences whether a patient feels like they’re being spoken to or spoken at. For example, the “hide self-view” feature on Whereby allows both patients and practitioners to focus entirely on the other person, reducing self-consciousness and making the interaction feel more natural and attentive.
When platforms are designed to reduce friction, minimize distraction, and reinforce human cues, clinicians can focus on listening, and patients can focus on being heard.
Measuring trust in virtual care experiences
The results of designing for patient trust show up clearly in product and operational metrics. Well-designed telehealth experiences will reduce friction, increase confidence, and create measurable improvements across patients, practitioners, and platform teams. Here’s how;
For patients, trust is reflected in outcomes like reduced no-show rates, faster time to appointment, and higher repeat usage of virtual visits. This is because when joining and participating in sessions feels reassuring, patients are more likely to show up and engage.
For practitioners, trust surfaces through higher satisfaction and quality scores for the platform. Since calm and reliable in-call experiences allow clinicians to focus on care rather than troubleshooting, it generally improves both perceived and actual care quality.
For telehealth and platform teams, strong trust signals translate into fewer support tickets, lower operational overhead, and reduced churn. For example, when Nilo switched its video call solution to Whereby, they recorded a 60% drop in technical support tickets. This shows that when the experience “just works,” issues are prevented rather than escalated.
By defining and tracking these trust indicators, teams can move beyond intuition and clearly connect design decisions to clinical outcomes and business performance.
Key Takeaways
In virtual care, trust is established long before a provider says hello. It’s built when the platform works, the experience feels familiar, and nothing unexpected happens.
For designers, this comes down to three actionable priorities:
Simplicity: Reducing cognitive load by not overcomplicating the user journey.
Transparency: Especially around sensitive moments like recording and transcription.
Accessibility: Making virtual care very inclusive for everyone and treating it as a responsibility, not a compliance checkbox.
Designing the future of virtual care won't be about more features. Instead, the user experiences will need to feel less like standalone calls and more like cohesive, supportive virtual care.
At Whereby, our telehealth experience is intentionally simple, browser-based, and designed to focus on the session. For teams who want tailored virtual care journeys, our video call API incorporates features and a UI proven to support trust, clarity, and ease of use.