How To Optimise Telehealth UI & UX for Better Patient Experience
Based on our extensive conversations with PMs across leading telehealth platforms, these are the 8 areas to optimize in telehealth UI and how to reframe your approach

Product Managers in telehealth carry a massive responsibility: delivering technology that doesn’t just function but enhances clinical outcomes, improves patient retention, and drives engagement. Yet, too often, telehealth video platforms focus on reliability, compliance, and UX fundamentals, missing critical opportunities to make virtual care more human-centered, intuitive, and impactful.
With 88% of users abandoning apps after a bad experience, a great user experience has never been more important. Not only can a better experience decrease churn and frustration for users but it can also play a large factor in increasing trust in telehealth overall and in turn result in better clinical outcomes. All of this alongside rising expectations from patients and practitioners alike make now the perfect time for Product Managers to reconsider and prioritise the UI and UX of their telehealth and virtual care offerings.
Based on our extensive conversations with PMs across leading telehealth platforms, here are the 8 areas where traditional thinking often falls short, and how to reframe your approach.
1. Video Consultations Aren’t Just “Virtual Visits”
The Challenge: Treating video consultations as digital replicas of in-person visits.
Unlike during an in-person visit, where the setting naturally fosters trust, patients log into a digital space that can feel cold, impersonal, and transactional if not designed intentionally.
Creating a seamless telehealth experience requires looking beyond technical stability and focusing on curated patient interactions. This means designing for comfort and trust - whether through personalized waiting rooms, intuitive onboarding flows, or UI elements that reduce patient anxiety. Small design choices can significantly impact how patients feel before, during, and after their consultation.
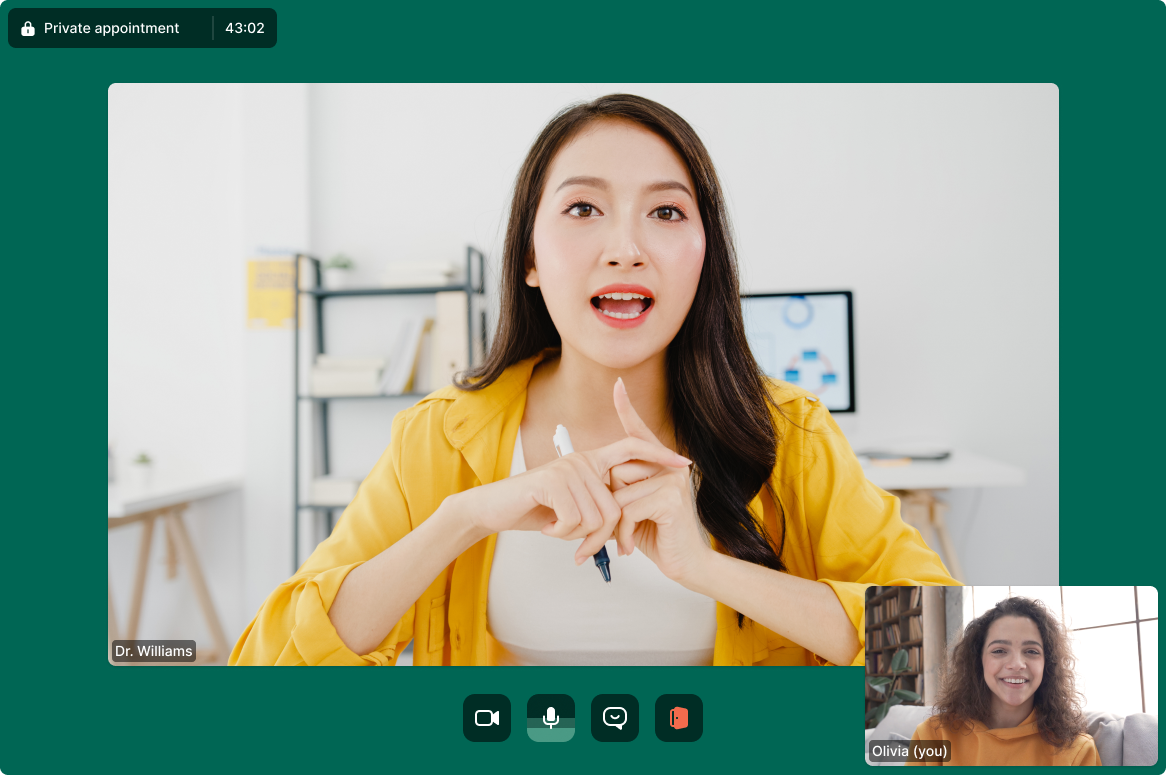
2. Video Layouts Are Killing Human Connection
The Challenge: Defaulting to rigid, grid-based layouts designed for business meetings and not patient care.
Trust is built visually, and video layouts dictate the patient-clinician connection. Yet, many platforms force participants into distracting, inefficient formats that break the flow of conversation.
Designing effective video layouts requires careful consideration of visual hierarchy and engagement mechanics. Should patients see themselves, or does hiding self-view improve focus? Would spotlighting the doctor foster a more natural interaction? How does the layout adjust across different devices? These choices go beyond UI tweaks as they shape trust, comfort, and communication quality.

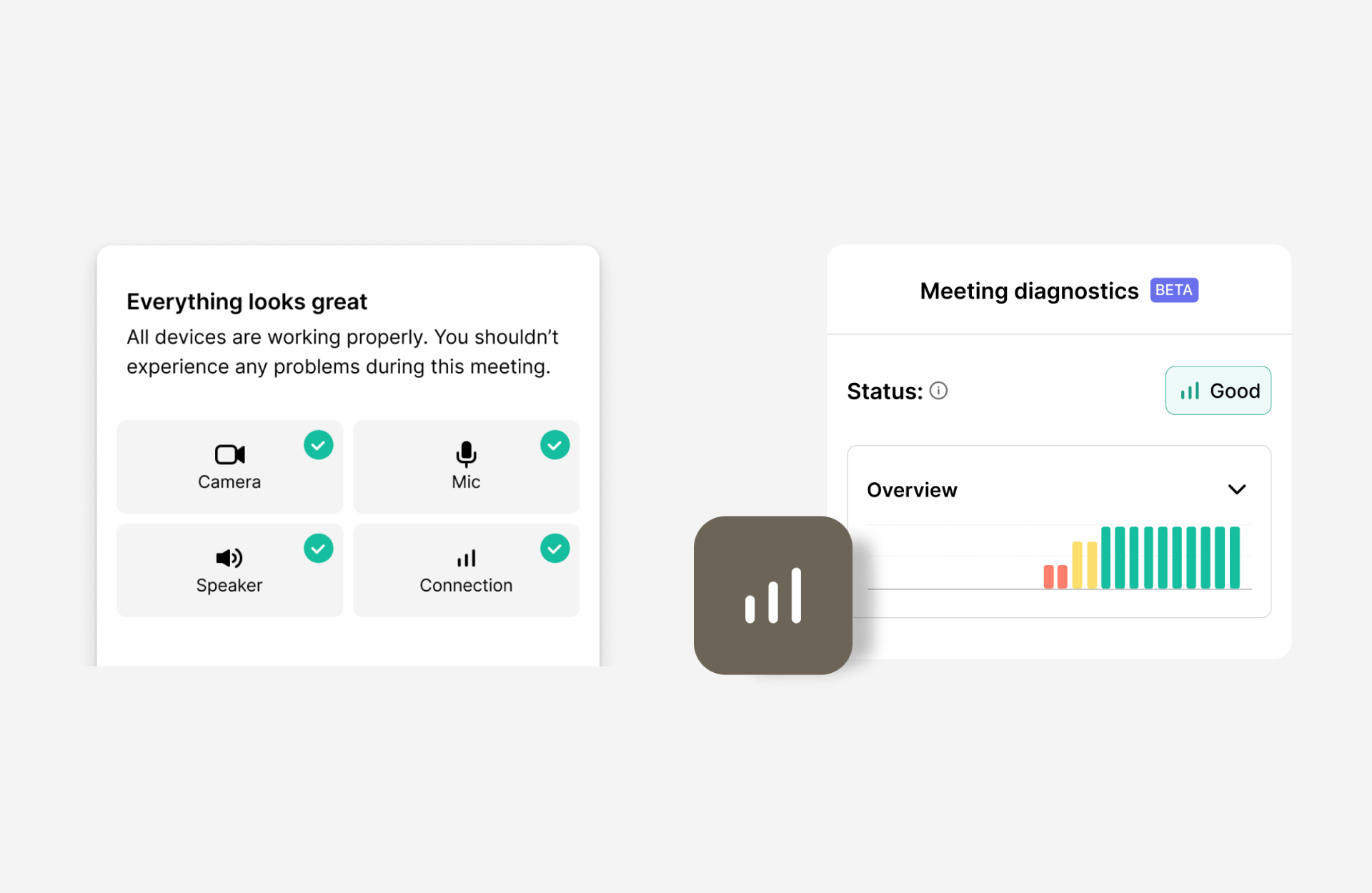
3. The Invisible Fatigue Factor
The Challenge: Underestimating video fatigue’s impact on both patients and clinicians.
Patients and providers don’t just experience fatigue from long calls. It’s also the cognitive load of poor interfaces, awkward eye contact, and unnatural interactions.
Minimizing video fatigue requires lightweight, low-latency video, thoughtful UI elements, and intuitive workflows. Pre-call diagnostics, in-call troubleshooting, and reducing unnecessary clicks help make virtual consultations feel fluid and effortless, rather than exhausting.
4. The Missed Opportunity of Post-Consultation Continuity
The Challenge: Thinking the patient experience ends when the call does.
What happens after a video call is just as important as what happens during it. If a patient logs off without clear next steps, adherence plummets.
Ensuring continuity in telehealth requires more than just a well-executed consultation. Automatic transcriptions, integrated scheduling for follow-ups, and seamless EHR updates help maintain patient engagement. The goal? Every consultation should drive a clear next step, reinforcing continuity of care and improving health outcomes.
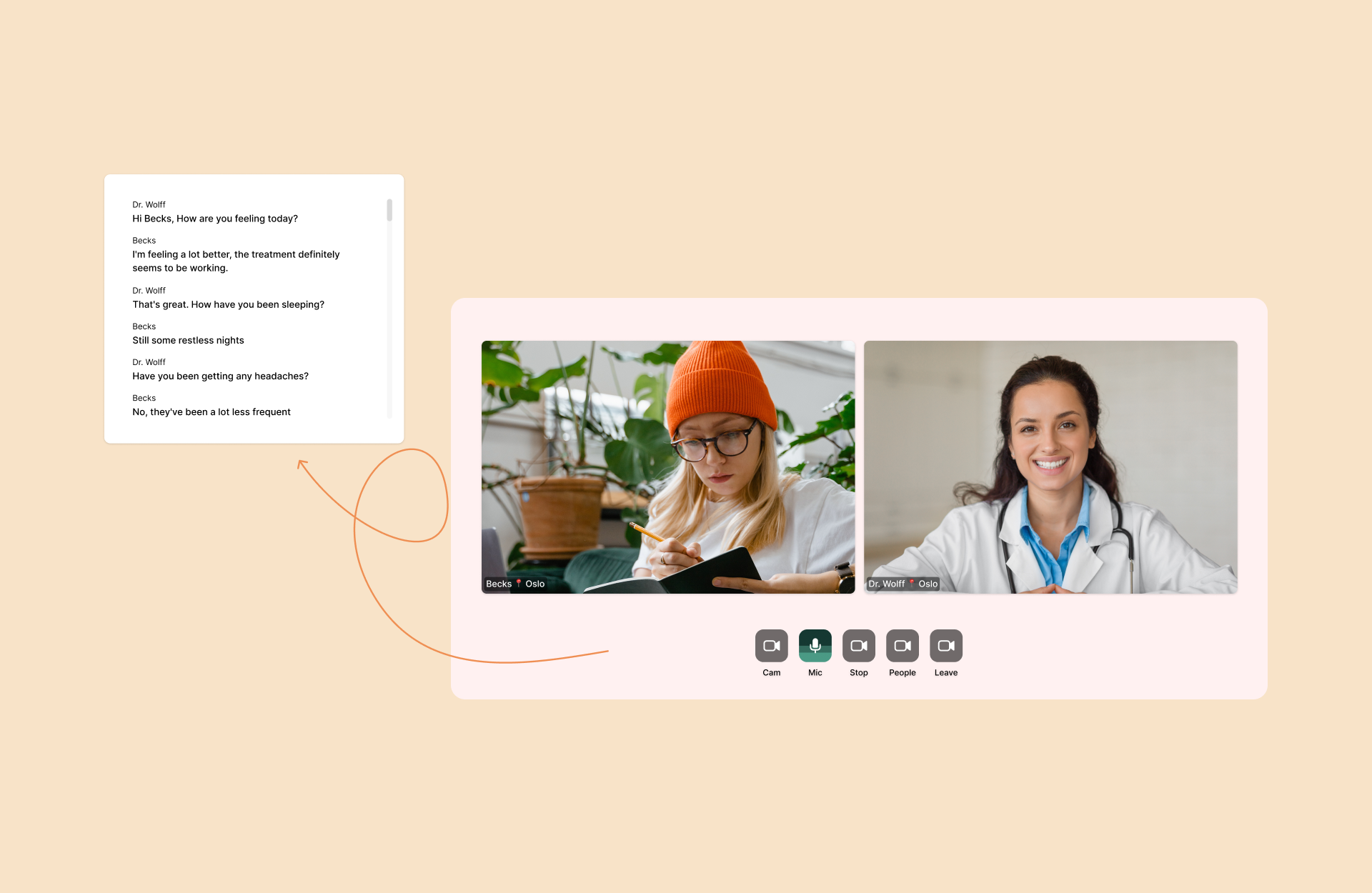
5. Accessibility Isn’t Optional
The Challenge: Treating accessibility as a compliance checkbox rather than a core UX principle.
Too many telehealth platforms view accessibility as a regulatory burden instead of an opportunity to drive adoption, engagement, and differentiation. True accessibility means frictionless experiences for all users - including those with disabilities, non-native speakers, and people with limited digital literacy.
Embedding real-time closed captions and customizable UI elements ensures accessibility for diverse patient needs without adding complexity. Thoughtful design choices create a more inclusive experience, removing barriers to care for individuals with a wide variety of needs.
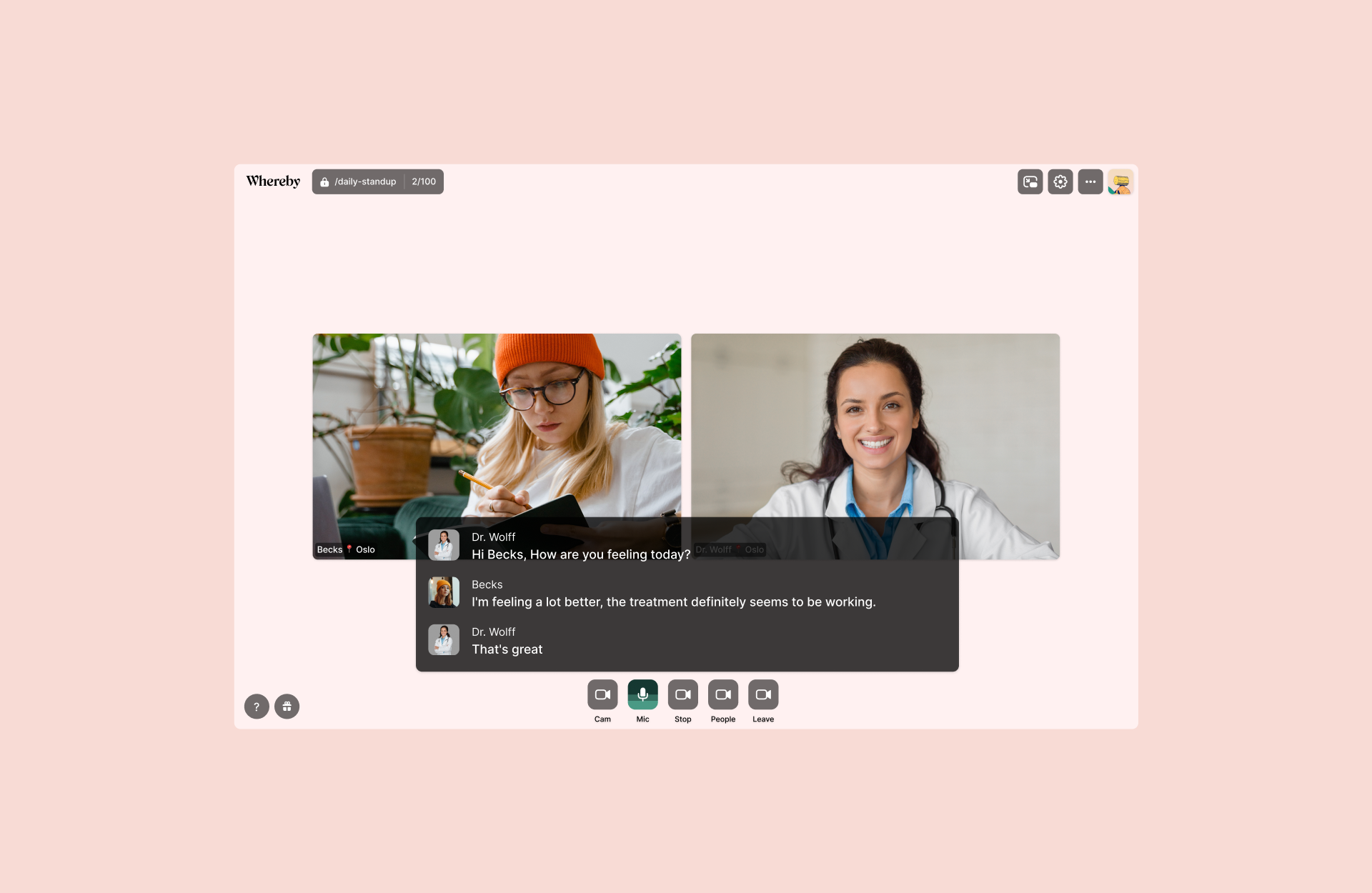
6. Privacy Isn’t Just a Legal Obligation
The Challenge: Thinking about privacy purely as a security measure, not a trust-building tool.
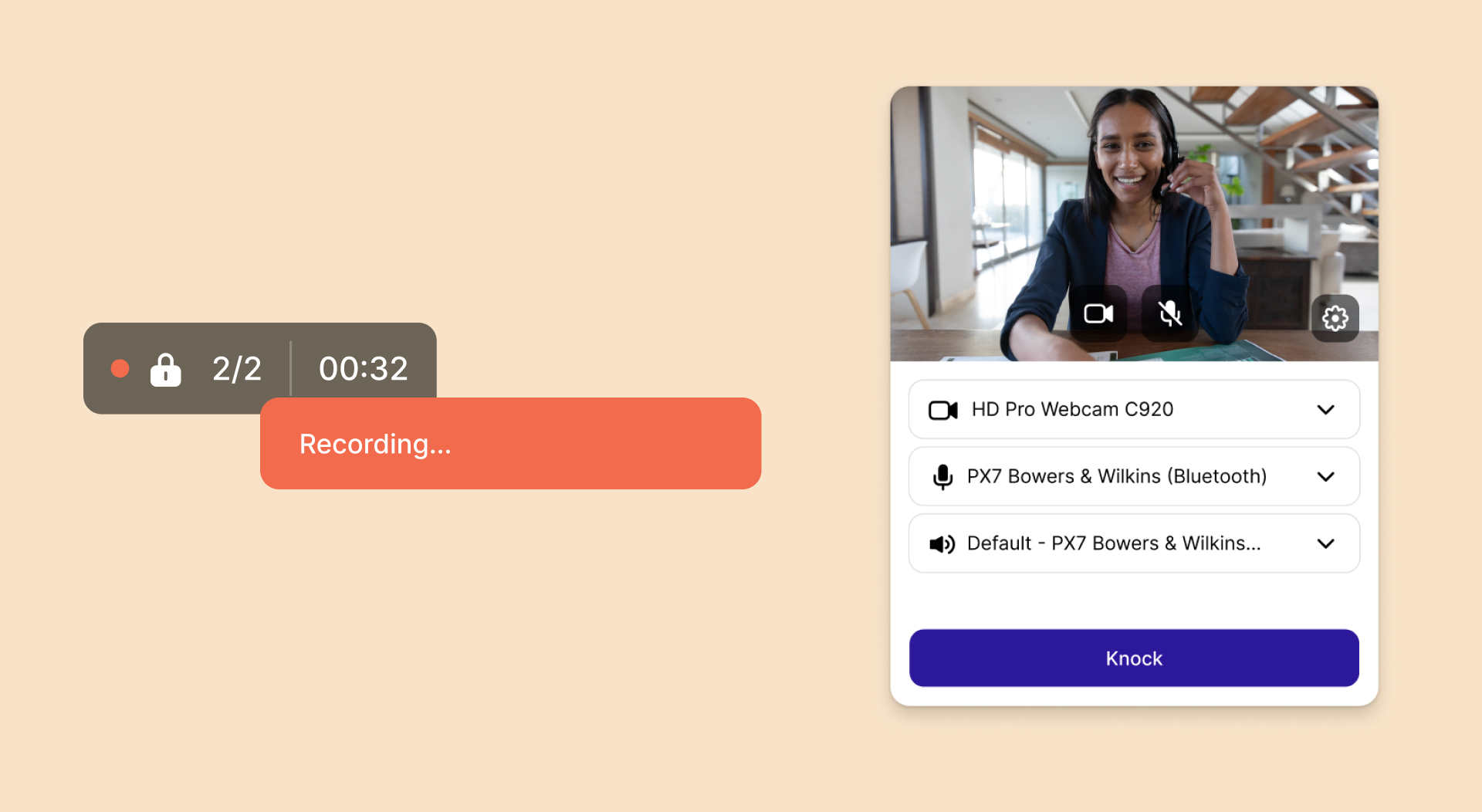
Patients expect compliance with HIPAA and GDPR, but compliance alone doesn’t build trust. Users want visible indicators that reinforce their control over their data.
Seamless privacy integration within the UI such as clear recording notifications, explicit participant lists, and consent-driven data handling fosters trust and confidence. When transparency is visible and intuitive, patients feel more secure in their virtual care experience.
7. First Impressions Drive Retention
The Challenge: Underestimating the impact of onboarding, UI flow, and first-time user experience.
A poor first interaction with a telehealth platform can lead to drop-offs, lower repeat usage, and frustrated clinicians.
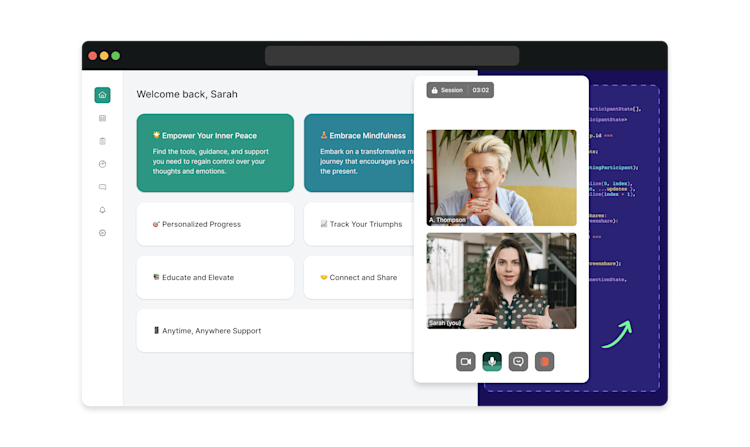
Onboarding should be designed with consumer usability in mind - streamlining access, reducing setup friction, and ensuring every click adds value. Patients should never struggle to join a session or navigate the platform, as ease of access directly impacts engagement and retention.
8. Build vs. Buy: The Smart PM’s Roadmap Decision
The Challenge: Hesitating to leverage third-party solutions that accelerate time-to-market.
Every telehealth product team faces the build vs. buy decision. Many default to building in-house without fully evaluating the opportunity cost - slower feature delivery, maintenance burdens, and stretched engineering teams.
Leveraging trusted external partners for complex infrastructure - such as video or scheduling - frees teams to focus on innovation and differentiation rather than foundational functionality.
Final Thought: The Best Telehealth Experience is Invisible
A truly exceptional telehealth experience is defined by care that feels seamless, connected, and intuitive. When technology fades into the background, patients and providers can focus on what really matters: meaningful, stress-free interactions that foster trust and better health outcomes.
By prioritizing empathy, trust, and usability, telehealth platforms not only enhance engagement, but they set a new benchmark for patient-centered digital care.
Find out more about Whereby’s telehealth video call API and discover how it can improve user experience on your platform.


