The Hidden Cost of “Good Enough” Technology in Virtual Care
In virtual care, what feels like a safe decision is often quietly accumulating risk, cost, and lost opportunity. Here's how this happens and why you should reconsider sticking with a 'good enough' solution.

For many healthcare teams, the video call solution and other tech stack often falls into a category where it’s not great, but it’s also not broken enough to switch immediately.
Switching feels risky and expensive, especially when there’s always another priority competing for attention.
But the truth is that in virtual care, what feels like a safe decision is often quietly accumulating risk, cost, and lost opportunity.
In this post, we’ll explain how exactly this piles up and why you should reconsider sticking with a suboptimal solution.
The real cost of settling for “good enough” tech in virtual care
The most dangerous costs aren’t always obvious line items on a budget. They’re the slow, compounding effects that show up months or years later. Here’s how they show up in telehealth.
1. Patients and clinicians quietly lose trust when there’s frequent reliability issues
Frozen screens, poor audio, or confusing workflows don’t always trigger alarms internally, but patients and clinicians often remember them.
Over time, these frustrations show up as low patient satisfaction scores, an increase in technical support tickets, and churn to other telehealth providers.
In virtual care, reliability is part of the clinical experience. And since expectations are high, especially when it relates to their healthcare, a solution that’s “mostly fine” today may not scale tomorrow.
2. Engineering teams pay for the migration cost daily
Oftentimes, the current solution works well enough because engineering teams have learned to work around its quirks. Sometimes, teams say they prefer to stick with the solution they know rather than risk any issues with a new provider.
What they don’t see is that these ‘good enough’ solutions often tend to require:
Custom workarounds and brittle integrations
Ongoing maintenance for features that should be native
Engineering time spent firefighting instead of innovating
These efforts compound. So every month spent maintaining a fragile system is a month not spent improving the care experience.
If the pain doesn’t come from ongoing maintenance, it comes from unexpected problems that disrupt the engineering roadmap. Primarily because teams have to drop everything else to find a fix.
Instead of spending engineering resources on launching new features or being innovative, it’s spent on maintaining or fixing an unforeseen problem with the existing solution.
Consider evaluating how much these recurring or one-off maintenance costs are and compare them to how much the team could have saved if you migrated earlier.
3. Compliance and security risks grow over time
Virtual care as we know it comes with regulatory, security, and privacy expectations that only increase over time. What feels “acceptable” today may become a serious liability as standards tighten and scrutiny increases.
When a team sticks with a tech stack that isn’t built for telehealth, they become exposed to security gaps that’ll surface during audits.
There’s also the last-minute compliance fixes whenever there’s a change in regulatory requirements, and most importantly, the growing risk that comes with scale.
4. Innovation is severely limited
Many digital health roadmaps depend on a solid foundation. At Whereby, this comes in the form of our reliable video infrastructure. Having a solid foundation allows flexibility and makes it easier to roll out new features (guided quarterly by our customers’ requests).
Most telehealth providers want to focus on more personalized care journeys, AI-assisted clinical workflows, and new care models.
But if the underlying infrastructure requires several workarounds and cannot support these new features, it automatically stifles innovation. The focus shifts to finding ways not to break the system, rather than being innovative in care delivery.
Your video call provider should be a tier-1 vendor that enables new care models and workflows to deliver actual value, instead of becoming another fragile layer in an already complex system.
5. Compounding frustrations lead to silent churn
Teams relying on a “good enough” virtual care setup often don’t see immediate churn because patients and clinicians don’t complain loudly or cancel overnight.
The technology works most of the time, but small issues like an unstable connection or device compatibility issues start to add up.
People still show up, but with less enthusiasm. Clinicians are less eager to schedule virtual visits, and patients are less likely to rebook. Virtual care usage becomes more inconsistent, even though nothing appears “broken.”
Engagement and confidence drop long before anyone actively decides to leave for a better alternative. The silent churn is a result of these multiple bad experiences.
6. Competitors capture the churn you don’t see
While one team waits for the “right time,” others are investing in a more reliable virtual care experience.
Teams with strong, dependable video solutions make onboarding easier, consultations smoother, and virtual care feel routine rather than risky. Clinicians trust the platform, and patients feel comfortable coming back.
When patients and clinicians start comparing options, those differences matter because a platform that “usually works” struggles against one that consistently does.
Over time, the differences between reliable virtual care and a ‘good enough’ one become harder to ignore. So when patients and clinicians have a choice, they naturally gravitate toward the platforms that feel more professional, dependable, and easier to use.
7. Stagnation becomes the default
Many telehealth platforms scaled during the pandemic, then saw their growth slow down because their infrastructure wasn’t built to support the next phase.
Some platforms continued to grow by partnering with a reliable, scalable video provider like Whereby. With a strong foundation in place, they could focus on expanding care and improving experience instead of fixing what was already live.
In a market where virtual care is no longer new, long-term growth favors platforms that remove infrastructure limits rather than work around them.
So partnering with a solid tier1 video call vendor increases your chances of long-term growth and scalability.
8. Delaying the decision to switch usually means rushing it later
Most virtual care teams don’t actively decide not to switch technology. What usually happens is that they decide to wait for the right time or for something to go wrong.
At first, the reasoning is that ‘it’s not perfect, but it works well enough’. If interest surfaces, internal conversations start, and then it gets delayed when other priorities take over.
Eventually, when teams are finally forced to act, the timeline is no longer theirs to control. What could have been a thoughtful, low-risk evaluation becomes a rushed transition under pressure.
Ideally, if you believe a change is likely in the next 12 months, the lowest-risk move is to start evaluating now. Early evaluation doesn’t mean early commitment; it creates options.
It gives teams time to understand migration effort, test assumptions, and move deliberately, rather than being pushed into a decision when “good enough” stops being good enough.
It’s time to switch to a better video call solution
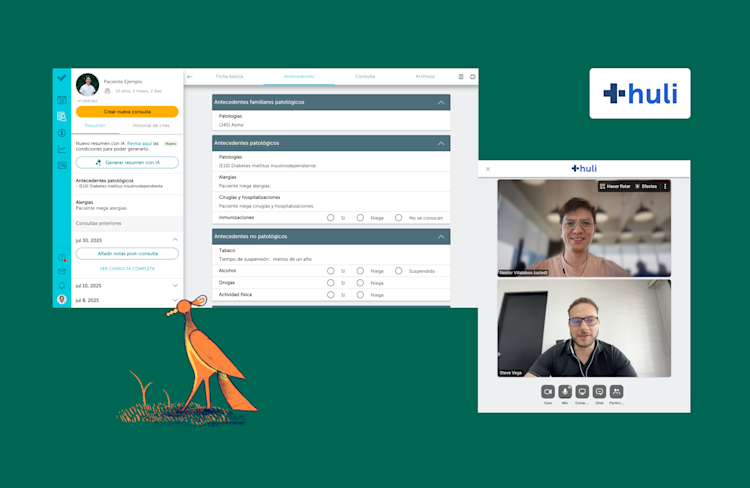
Whereby enables digital health teams to embed secure, reliable video consultations directly into their product without the traditional heavy lifting of building and maintaining video infrastructure.
Built specifically for telehealth with over a decade of WebRTC experience, our video call API is guided by our global healthcare customers like Jane, Unobravo, Tebra, Accurx, and more, whose feedback directly shapes our roadmap.
Most telehealth teams often start small, launching a proof of concept in hours, then fully embedding and customizing over a few weeks.
Larger organizations often take a phased approach. They begin with a limited pilot, roll it out to a test cohort, and then gradually migrate more users onto Whereby. This allows teams to prove viability, gather real-world feedback, and give clinicians and patients time to adjust to the new experience.
If you’re completely confident in your current setup, that’s great. But if there’s even a hint of doubt about whether your video stack will scale over time, it may be worth evaluating another solution.
Find out more about how Whereby works.